Abstract

Background: Current literature recommends 28-day cycles of a hypomethylating agent (HMA) with continuous daily venetoclax (Ven) in select patients with newly diagnosed acute myeloid leukemia (AML). Key adverse events observed with azacitidine-Ven were grade ≥ 3 thrombocytopenia, neutropenia, and febrile neutropenia. Emerging data recommends HMA-Ven in relapsed/refractory (r/r) high-risk myelodysplastic syndrome (MDS) with a Ven duration ranging from 14-28 days of a 28-day cycle. Predominant grade ≥ 3 treatment emergent adverse events (TEAEs) also included cytopenias in this patient population. As the combination of HMA-Ven for patients with MDS and AML is increasingly utilized, practice variations in the initial duration of Ven requires evaluation. This study aims to characterize the safety profile with continuous or modified duration Ven after complete remission (CR), complete remission with incomplete hematologic recovery (CRi) or cycle 3 to further assess the safety profile of HMA-Ven due to treatment instead of disease.
Methods: This is a retrospective, single center study of patients > 18 years of age with AML or MDS receiving HMA-Ven between December 1, 2017 - January 31, 2021. Patients were excluded if enrolled in an investigational protocol or received therapy at an outside hospital. To capture treatment-related neutropenia, thrombocytopenia, and other safety endpoints, patients were excluded if they received < 3 cycles of HMA-Ven, as cytopenias could be due to disease burden. Data was collected from day -21 until the completion of cycle 6 or last completed cycle. The primary end point was grade > 3 neutropenia for > 7 days. Secondary endpoints included grade > 3 anemia or thrombocytopenia for > 7 days, incidence of febrile neutropenia, antimicrobial use, dose interruption or delay, dose or duration modification, therapy discontinuation, and assessment of CR and CRi. Descriptive statistics were utilized to describe outcomes and safety endpoints were graded with the Common Terminology Criteria for Adverse Events, version 5.0 (CTCAE v.5.0).
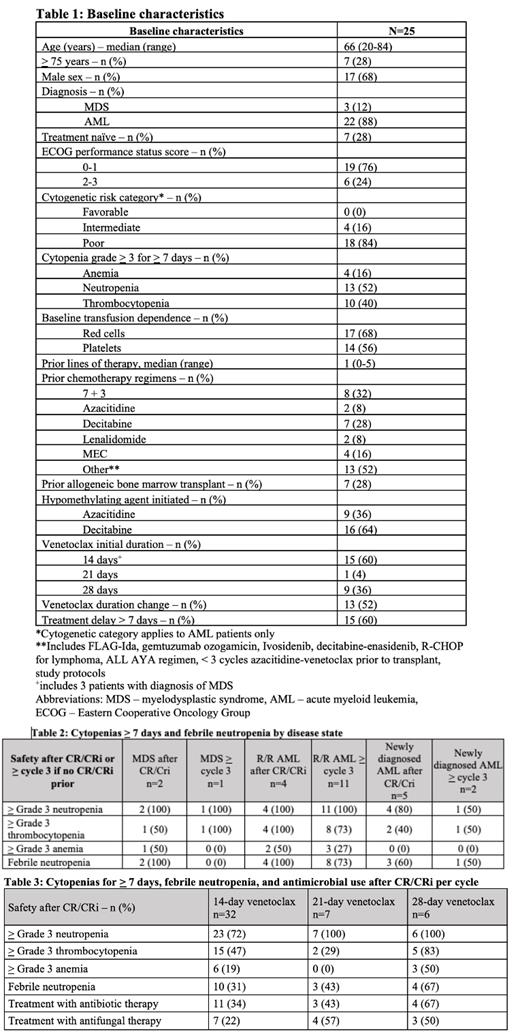
Results: 25 patients were included in analysis. The median age was 66 years (range 20-84) and 12% (n=3) had a diagnosis of MDS while 88% (n=22) had a diagnosis of AML. Most patients with AML had poor cytogenetic risk (n=18, 84%) and 28% (n=7) were treatment naïve. Prior therapies are outlined in Table 1. Ven was initiated with a 14-day duration in 60% (n=15) of patients, including 3 patients with MDS, 4 patients with r/r AML, and 4 patients with r/r AML with a prior allogeneic transplant. Many patients required a subsequent duration change of Ven throughout the evaluation period (n=13, 52%). Treatment delays of > 7 days occurred in 60% (n=15) of patients. 12 patients (48%) achieved CR or CRi and accounted for 45 evaluated cycles. Of the 12 patients, 4 started with 28-day ven, 1 with 21-day, and 7 with 14-day. Of the patients who achieved CR or CRi, there were 32 cycles with Ven 14-day durations, 7 cycles with 21-day duration, and 6 cycles of 28-day duration. Grade 3 or higher neutropenia for > 7 days was observed in 72% (n=23) of the 14-day durations and 100% of the 21-day and 28-day Ven durations. Grade 3 or higher thrombocytopenia and anemia was most common in the 28-day duration Ven at 83% (n=5) and 50% (n=3), respectively. Febrile neutropenia and treatment with antibiotic therapy had higher incidence of 67% (n=4) in the 28-day Ven duration. Most patients received treatment with antibiotic therapy (75%, n=9) and antifungal therapy (67%, n=8) after achieving CR or CRi on HMA-Ven. In those with newly diagnosed AML, 29% (n=2) and 57% (n=4) achieved CR and CRi respectively. 67% (n=2) of the MDS patients and 27% (n=4) of the r/r AML population achieved CRi. Of the 9 patients with prior HMA exposure, 2 patients achieved CRi.
Conclusions: There was a high incidence of grade 3 or higher cytopenias, but a trend toward increased neutropenia, thrombocytopenia, febrile neutropenia, and infectious complications were observed in those receiving a 21-day or 28-day Ven duration after CR or CRi compared to those receiving a 14-day duration of Ven. Early decreased durations of Ven and further decreases outside the prescribing information after patients are in CR may be a reasonable and safe option for patients who are not likely to tolerate continuous Ven, such as those with prior MDS, r/r disease, or patients who have received prior allogeneic transplant. This requires further investigation.
Lei: AbbVie: Honoraria; Epizyme: Honoraria; Intervention Insights: Consultancy; Fresenius Kabi: Consultancy. Brunner: GSK: Research Funding; Agios: Consultancy; Keros Therapeutics: Consultancy; AstraZeneca: Research Funding; Aprea: Research Funding; Acceleron: Consultancy; Janssen: Research Funding; Takeda: Consultancy, Research Funding; BMS/Celgene: Consultancy, Research Funding; Novartis: Consultancy, Research Funding. Fathi: Kite: Consultancy, Honoraria; Foghorn: Consultancy, Honoraria; Kura: Consultancy, Honoraria; Trillium: Consultancy, Honoraria; Genentech: Consultancy, Honoraria; Daiichi Sankyo: Consultancy, Honoraria; Astellas: Consultancy, Honoraria; Seattle Genetics: Consultancy, Honoraria; Blueprint: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; Celgene/BMS: Consultancy, Honoraria, Research Funding; Servier: Research Funding; Agios: Consultancy, Honoraria, Research Funding; AbbVie: Consultancy, Honoraria, Research Funding; Morphosys: Consultancy, Honoraria; Ipsen: Consultancy, Honoraria. Signorelli: Bristol Myers Squibb: Consultancy; AbbVie: Honoraria.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal